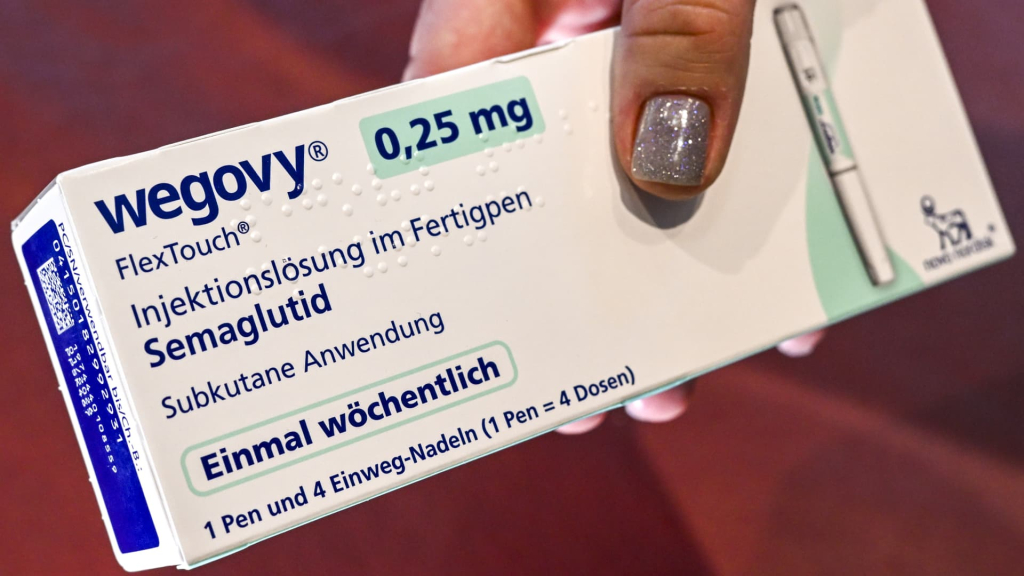
CVS Health announced on Thursday a major initiative to enhance accessibility to the popular weight loss medication Wegovy through its pharmacy benefit manager, Caremark.
Effective July 1, Caremark will feature Wegovy prominently on its formularies—select lists of covered medications—designating it as the preferred GLP-1 treatment for obesity. This change results from a new collaboration between Caremark and Wegovy’s creator, Novo Nordisk, as outlined in CVS’ quarterly earnings report.
As part of this shift, Caremark will remove the weight loss drug Zepbound from its standard formularies, a decision that impacts its manufacturer, Eli Lilly, according to a CVS spokesperson speaking to Finance Newso. These standard formularies are utilized by the majority of Caremark’s clients, representing millions of patients nationwide.
Patients who are currently prescribed Zepbound and are covered by Caremark will be eligible to transition to Wegovy, the spokesperson noted.
The announcement led to a 1% rise in Novo Nordisk’s shares on Thursday, while Eli Lilly’s stock experienced an 8% decline.
This development comes as Novo Nordisk seeks to enhance Wegovy’s availability, now that supply issues in the United States have been resolved. Partnering with Caremark, one of the largest pharmacy benefit managers in the country, is viewed as a strategy to reach a wider patient population.
Caremark serves as an intermediary, negotiating drug prices with manufacturers on behalf of insurance companies and creating lists of medications—formularies—that are reimbursed at pharmacies.
Under the new agreement, Caremark will provide Wegovy at a more affordable price for its members. The pharmacy benefit manager has successfully negotiated a more favorable net price for Wegovy compared to Zepbound, resulting in cost savings for clients that choose those formularies, according to the CVS spokesperson.
However, clients of Caremark, which include various employers and unions, will individually determine how much of the savings on Wegovy is passed on to their members, either through reduced premiums or lower copays at the pharmacy.
For those lacking insurance coverage for Wegovy or any other GLP-1 drugs, patients can purchase Novo Nordisk’s medication out-of-pocket for $499 at any of CVS’s 9,000 pharmacies across the country, the spokesperson indicated.
CVS further revealed in its earnings report that it has become the first retail pharmacy to collaborate with Novo Nordisk’s new direct-to-consumer online service, NovoCare, to supply Wegovy to patients with prescriptions. NovoCare aims to offer the drug at this lower price point to cash-paying customers who may find it challenging to manage the typical list price of approximately $1,000 without insurance and other discounts.
Additionally, Caremark plans to offer Wegovy alongside supplementary lifestyle strategies, including personalized nutrition plans, as part of its CVS Weight Management program.
This announcement arrives at a time when Novo Nordisk is keen to extend its patient reach, particularly as many compounding pharmacies face legal restrictions on producing cheaper, unapproved variants of Wegovy, with few exceptions.
CVS Health Group President Prem Shah remarked during an earnings call, “It’s unclear how the transition from compound pharmacies to other pharmacy settings will unfold. However, we anticipate significant advantages in providing 9,000 locations for patients to access their medications.”
In a separate statement, Dave Moore, Novo Nordisk’s Executive Vice President of U.S. operations, emphasized the company’s commitment to collaborating with various stakeholders in the U.S. healthcare system to discover innovative solutions that fulfill patient needs and connect them with authentic, FDA-approved Wegovy in a convenient and affordable manner.